Traumatic dental injury. Crown and root fractures. Soft tissue injury
TOOTH CROWN FRACTURE
Tooth crown fracture involves smaller or larger part of the tooth crown which has broken off and it may result the tooth nerve (pulp) to be exposed.
Immediate Action in the Accident Site
- Find the broken tooth fragment and put it into the saline solution, pasteurised milk, or victim´s saliva.
- Do not clean the tooth with spirits or other disinfectants.
- See a dentist. It is often possible to reinstate the broken tooth fragment into the mouth.
If you see a pink spot on the fracture site or bleeding inside the tooth, the pulp tissue could be exposed and emergency treatment is necessary (covering the tooth nerve and tooth restoration). The tooth may become very sensitive and the tooth nerve may be permanently damaged, root canal treatment may be required (see patient information for Root canal treatment).
Follow-up visits: 2-4 weeks, 6-8 weeks, 3 kuud, 6 months and one year after trauma.
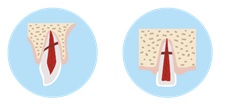
DENTAL ROOT FRACTURE
Dental root fractures are undetected by the patient. This is diagnosed by radiographic imaging at the dental office.
Immediate Action at the Accident Scene
- Gently bite down on a napkin/gauze to leave it sit between damaged upper and lower teeth.
- See a dentist as soon as possible.
Further prognosis and treatment depends on the position of the fracture line. It may be possible to fix the tooth fragment with a splint. Root canal treatment up to fracture line may be performed if necessary (see patient information for Root canal treatment).
Follow-up visits: 2 weeks, 4 weeks, 6-8 weeks, 4 months, 6 months and one year after trauma, then once a year for the following 5 years.
SOFT TISSUE INJURY
Facial injuries may also involve the soft tissues damage (gums, lips, skin). You may notice hematomas and wounds inside the mouth or around it. Sometimes a tooth fragment may migrate into the soft tissue.
Actions at the scene of accident:
- Remain calm. If you are providing help, calm the injured person.
- Carefully clean the abrasions and wounds with water.
- Carefully press a clean gauze or napkin on the injured area to stop the bleeding.
- Soft tissues of the oral cavity bleed heavily and injury may appear more severe. See a doctor for a wound management if necessary.
- Ensure that teeth are not injured or changed their position. Check that the tongue is intact. If a tooth has dislodged or broken tooth fragment is present, try to locate it. Only grasp the crown (wilder part of tooth).
- If the bleeding is under control and there are no other injuries, please see a dentist for further examination and treatment recommendations.
Please note: If you experience facial trauma outside of appointment hours of dental practice please attend the emergency department in order to receive emergency treatment. In case of extensive injuries call an ambulance or go to the emergency department immediately.
POSSIBLE COMPLICATIONS AFTER DENTAL TRAUMA
The most common complications are dental pulp necrosis (death of the tooth nerve), inflammation of the root apex area, root destruction (resorption) or replacement by bone (ankylosis), change in tooth colour or position, gum recession. Tooth ankylosis in childhood contributes to the developmental delay of the jaw in the trauma area and later orthodontic/surgical treatment is necessary. Unfortunately, it is not always possible to save your tooth, but with timely management, treatment is successful. Always see a dentist after a dental trauma. Schedule follow up visits regarding the traumatised tooth after your visit. Visit your dentist again if the tooth becomes sensitive, more mobile, changes colour (pinkish, yellowish, greyish) or if gingivitis develops. It is recommended to use individual mouth guards made by your dentist when playing sports to prevent dental trauma.
HOME CARE AFTER DENTAL TRAUMA
- Kindly avoid sports and physical exercise following the trauma in the mouth.
- Eat soft foods in the next two weeks and avoid biting and chewing on hard substances. It is recommended to chew with the opposite side of the mouth.
- Maintain excellent oral hygiene: brush teeth twice daily with a soft toothbrush and fluoride-containing toothpaste; clean contact surfaces of uninjured teeth with dental floss and interdental brush. As a result of poor oral hygiene, gingivitis may occur and worsen the prognosis of treatment.
- Especially maintain the proper oral hygiene of the injured area! During the first week, it is recommended to perform oral hygiene procedures after each meal.
- If the teeth were immobilized with the splint, carefully clean the area around it with interdental brushes and dental floss. Visit the dentist after 2-4 weeks to remove the splint.
- Don’t touch the traumatised area with your tongue or fingers.
- Rinse your mouth with chlorhexidine mouthwash twice a day for 1-2 weeks.
- Apply 0,2% chlorhexidine gel on the wound with a clean cotton or gauze pad 2-3 times a day.
- Take over-the-counter analgesics as necessary. Adults: 400 mg to 600 mg of ibuprofen and/or 500 mg to 1000 mg of paracetamol every 6 to 8 hours (or other over-the-counter analgesics). Please note: The pediatric dosage has to be adjusted according to their body weight.
- Antibacterial treatment is indicated for tooth avulsion (completely dislodged tooth from the socket) and soft tissue injuries.
If your condition worsens or you have any questions, please contact your dentist or healthcare provider.
Authors: Dr Valeria Hameury, Dr Teele Paltsar, Dr Marjo Sinijärv and Anna Firsova
2023